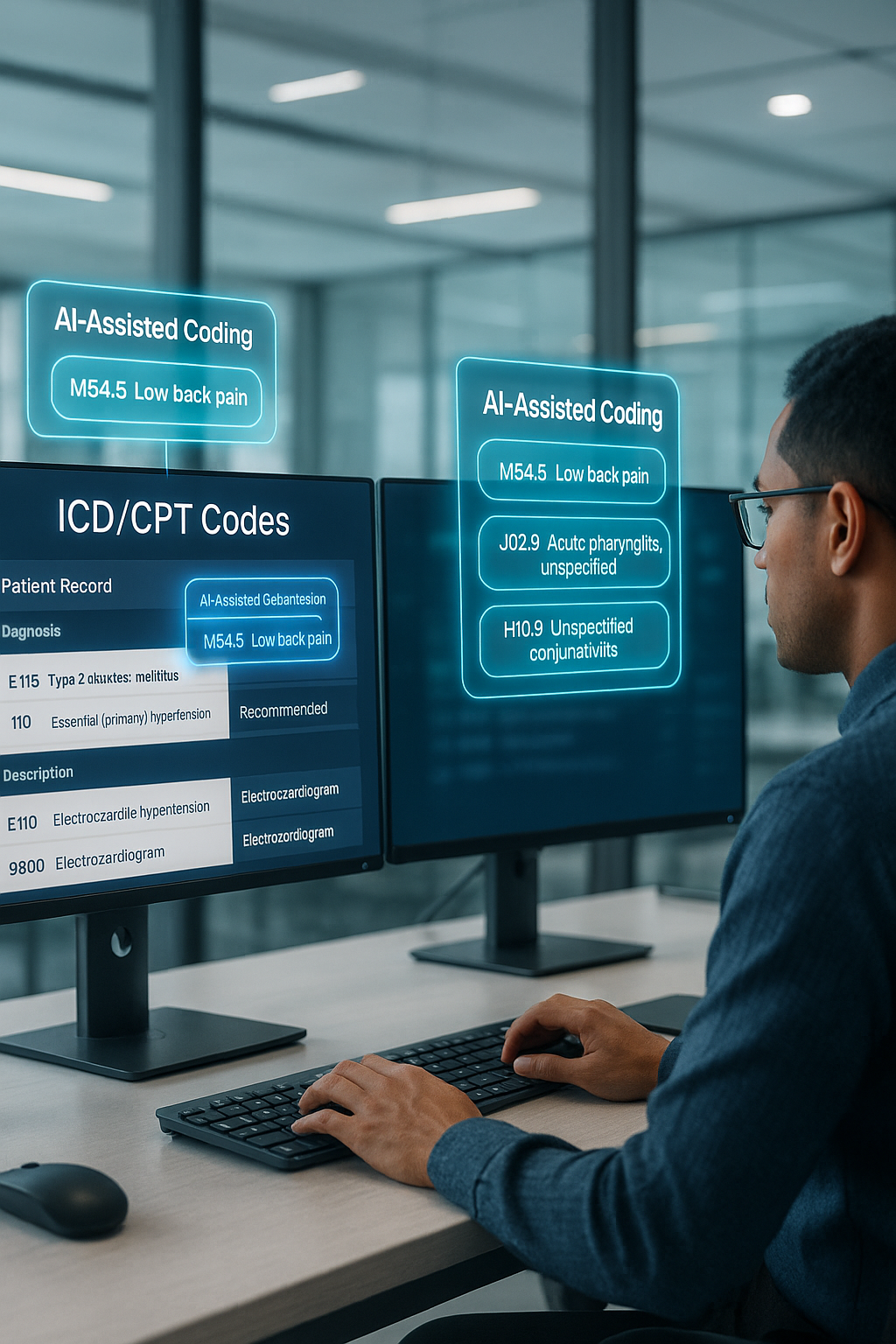
Accurate Medical Coding and Claims Processing to Maximize Reimbursements
At Zenexa Infotech, we provide comprehensive support across the entire claims management lifecycle, helping healthcare organizations reduce denials, improve cash flow, and stay compliant. Our certified medical coders — including CPC, CCS, and CRC professionals — are trained in ICD-10, CPT, and HCPCS standards, ensuring precise coding based on thorough clinical documentation.
From initial claims submission to denial tracking and follow-ups, we collaborate closely with your billing or RCM team to streamline workflows, minimize rework, and accelerate the payment process. Our coding services support multiple specialties and payer types, maintaining high accuracy and adherence to compliance guidelines.
Zenexa’s scalable approach is designed to boost clean claim rates, reduce administrative overhead, and shorten your revenue cycle without compromising on data integrity or regulatory standards.
Choose Zenexa Infotech to optimize your claims process with accurate coding and proactive claims management tailored to your organization’s needs.
See What Our Clients Are Saying
“We stopped losing money to small eligibility errors. Zenexa’s team feels like part of our own staff.”
“Finovate has been instrumental in our growth. Their team took the time to truly understand our needs and helped us eliminate inefficiencies.”
“Partnering with Finovate was a game-changer for us. They took the time to understand our challenges and helped us streamline our operations for success.”